Millions of people worldwide are affected by rheumatoid arthritis. While not lethal in itself, it is nothing short of devastating for sufferers. In severe cases, it can lead to serious deformities over the years. A recent experiment suggests that changing to a more plant-based may offer relief.
Changing your diet seems like a small price to pay for pain relief.
Read the full transcript below.
Rheumatoid arthritis is a chronic systemic autoimmune disease affecting millions, characterized by persistent pain and stiffness, and progressive joint destruction — particularly in the hands and feet, leading to crippling deformities. What can we do to prevent and treat it? In a famous 13-month-long randomized controlled trial of plant-based diets for rheumatoid arthritis, patients were put on a vegan diet for three and a half months and then switched to an egg-free lactovegetarian diet for the remainder of the study.
Compared to the control group that didn’t change their diet at all, the plant-based group had a significant improvement in morning stiffness within the first month, cutting the number of hours they suffered from joint stiffness in half. Pain dropped from five out of ten down to less than three out of ten. A drop in disability.
They reported subjectively feeling better, significant improvements in their grip strength in their hands, fewer tender joints, less tenderness per joint, and less swelling, with the added benefit of losing about 13 pounds and keeping most of that weight off throughout the year. They also had a drop in inflammatory markers in their blood, sed rate, C-reactive protein, white count.
The question is: “Why?”.
What does diet have to do with inflammatory joint disease? Well, rheumatoid arthritis is an autoimmune disease, in which your body attacks the lining of your own joints. Why would it do that? Well, there’s a different autoimmune disease called rheumatic fever, in which your body attacks your own heart.
Again, why would it do that? Well, it appears to be a matter of friendly fire. Rheumatic fever is caused by strep throat, which is caused by a bacteria that has a protein that looks an awful lot like a protein in our heart. So when our immune system attacks the strep bacteria, it also attacks our heart valves, triggering an autoimmune attack by “molecular mimicry.”
The protein on the strep bacteria is mimicking a protein in our heart, so our body gets confused and attacks both. That’s why it’s critical to treat strep throat early to prevent our heart from getting caught in the crossfire. So researchers thought maybe rheumatoid arthritis might be triggered by an infection as well. A clue to where to start looking was the fact that women seem to get rheumatoid arthritis three times more frequently than men. What type of infection do women get more than men? Urinary tract infections.
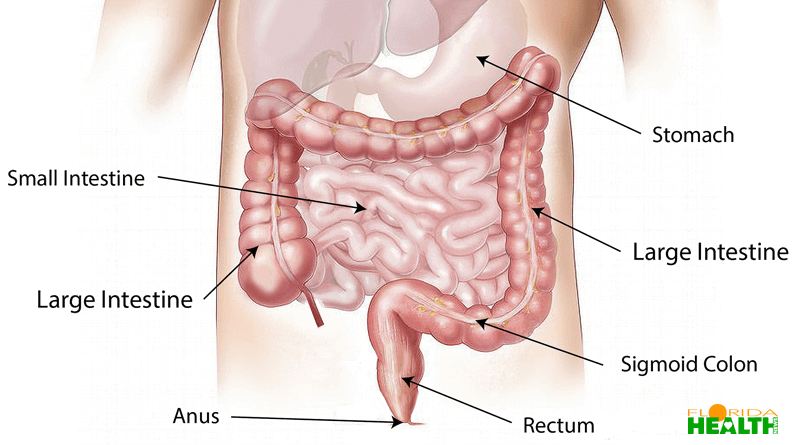
So researchers started testing the urine of rheumatoid arthritis sufferers and, lo and behold, found this bacteria called Proteus mirabilis. Not enough to cause symptoms of a UTI, but enough to trigger an immune response. And indeed there’s a molecule in the bacteria that looks an awful lot like one of our own molecules in our joints, so anti-Proteus antibodies against the bacteria may inadvertently damage our own joint tissues, leading eventually to the joint destruction. Therefore, therapeutic interventions aimed at the removal of this bacteria from the bodies of patients, with consequent reduction of antibodies against the organism should lead to a decrease in inflammation. Well, as we saw before, urinary tract infections originate from the fecal flora. The bugs crawl up from the rectum into the bladder.
And so how might one change the bugs in one’s colon? By changing our diet. Some of the first studies over 20 years ago in trying to fundamentally shift people’s gut flora were done using raw vegan diets, figuring that’s about as fundamental a shift from the standard Western diet as one can get. And indeed within days one could significantly shift someone’s gut flora. And you put rheumatoid arthritis sufferers on that kind of diet, and they experienced relief. And the greater improvements were linked to greater changes in their gut flora. But the diet was considered so intolerable that half the patients couldn’t take it and dropped out, perhaps because they were trying to feed people things like buckwheat-beetroot cutlets buttered with a spread made out of almonds and fermented coconut juice. Excuse me, not coconut; that might have been good.
Cucumber juice.
Thankfully regular vegetarian and vegan diets work too, changing the intestinal flora and improving rheumatoid arthritis. But we didn’t specifically have confirmation that plant-based diets brought down anti-Proteus antibodies, until now. Those that responded to the plant-based diet showed a significant drop in anti-Proteus mirabilis antibodies compared to the control group. Maybe it just dropped immune responses across the board? No, antibody levels against other bugs remained the same. So the assumption is that the veg diet reduced urinary or gut levels of the bug.
A shift from an omnivorous to a vegetarian diet has a profound influence on the composition of our urine, for example, higher levels of lignans in the urine of those eating vegetarian. Up until now it was just thought that they protected people eating more plant-based from getting cancer. But now we know lignans can also have antimicrobial properties as well so maybe helping to clear Proteus from our system. Either way, this suggests a new type of therapy for the management of rheumatoid arthritis. This new treatment includes anti-Proteus measures such as dietary manipulations in the forms of vegetarian diets.
While there may need to be additional research required, changing what you eat to include more greens and less meat seems like a small price to pay for the relief. When you add the additional benefits of eating more greens (weight loss, etc…) it becomes a no-brainer.

Carl Riedel is an esteemed online researcher and writer, specializing in the intersection of technology and wellness. As a member of the International Association of Therapists, Carl brings a unique perspective to his work, skillfully integrating insights from therapy and digital trends. His articles help readers navigate the complexities of the digital age with an emphasis on promoting mental and emotional well-being.